Alexander Disease
Overview
Alexander disease, an exceedingly rare neurodegenerative condition, typically emerges during infancy, categorizing it among leukodystrophies
Leukodystrophies is a collection of unusual genetic disorders impacting the brain's white matter.
Stemming from a mutation in the GFAP gene, responsible for encoding glial fibrillary acidic protein, Alexander disease distinctly affects astrocyte cells, rendering it a principal astrocytic disorder.
Alexander Disease Symptoms
• Developmental delays: Children with Alexander disease may face delays in achieving developmental milestones, including sitting up, crawling, or walking.
• Intellectual disability: The condition can lead to varying degrees of intellectual impairment, impacting learning abilities and cognitive development.
• Seizures: Individuals with Alexander disease may experience seizures of different intensities, ranging from mild to severe.
• Progressive neurological decline: Alexander disease typically results in a progressive loss of motor function, coordination difficulties, muscle stiffness (spasticity), and eventual loss of motor skills.
• Enlargement of the brain and head: Some cases may involve macrocephaly, an abnormal enlargement of the head due to the accumulation of fluid-filled spaces in the brain.
Causes & Risks of Alexander Disease
• Alexander disease arises primarily from mutations in the GFAP gene, responsible for producing glial fibrillary acidic protein crucial for astrocyte structural support in the brain.
• GFAP mutations result in faulty protein production, leading to the formation of protein clumps within astrocytes, disrupting their function.
• This disruption triggers white matter degeneration and the formation of Rosenthal fibers, characteristic of Alexander disease.
• The condition typically stems from new mutations and isn't inherited, categorized as a sporadic disorder occurring randomly.
• Its rarity and lack of familial patterns make defining risk factors challenging, though ongoing research aims to unravel genetic and environmental contributors.
• Currently, specific risks or environmental factors influencing Alexander disease development remain unidentified.
Test & Diagnosis
• Alexander disease diagnosis relies on clinical symptoms, brain imaging, and genetic testing for GFAP mutations.
• Clinical evaluation includes assessing neurological symptoms and developmental delays.
• Brain imaging reveals characteristic features indicative of Alexander disease.
• Genetic testing identifies mutations in the GFAP gene, confirming the diagnosis.
• Consulting healthcare professionals with expertise in neurological and genetic conditions is crucial.
• Accurate diagnosis and effective management require collaboration between patients, caregivers, and specialized medical teams.
Treatment
The treatment approach is centered around effectively managing the symptoms associated with the condition, closely monitoring the patient's condition. Some examples of treatment methods include:
• Using anti-seizure medication to control seizures.
• Physical therapy and baclofen to improve spasticity and hypertonia.
• Utilizing appropriately fitted equipment such as ankle braces to increase mobility.
• Treating obstructive hydrocephalus with a ventriculoperitoneal shunt.
• Working with a feeding specialist to improve malnutrition.
• Controlling reflux or vomiting with a proton pump inhibitor.
• Treating urinary retention and incontinence through bladder training, catheterization, and various medications.
Living With
Living with Alexander disease presents significant challenges, given its progressive impact on neurological function.
Individuals and their families grapple with various difficulties, including physical challenges that affect mobility and muscle control, necessitating assistive devices.
Communication hurdles may arise as the disease progresses, requiring speech therapy and alternative communication methods.
Managing medical and healthcare needs involves regular monitoring and coordination among healthcare professionals.
Cognitive impairments and developmental delays are common, necessitating tailored educational support.
Complications
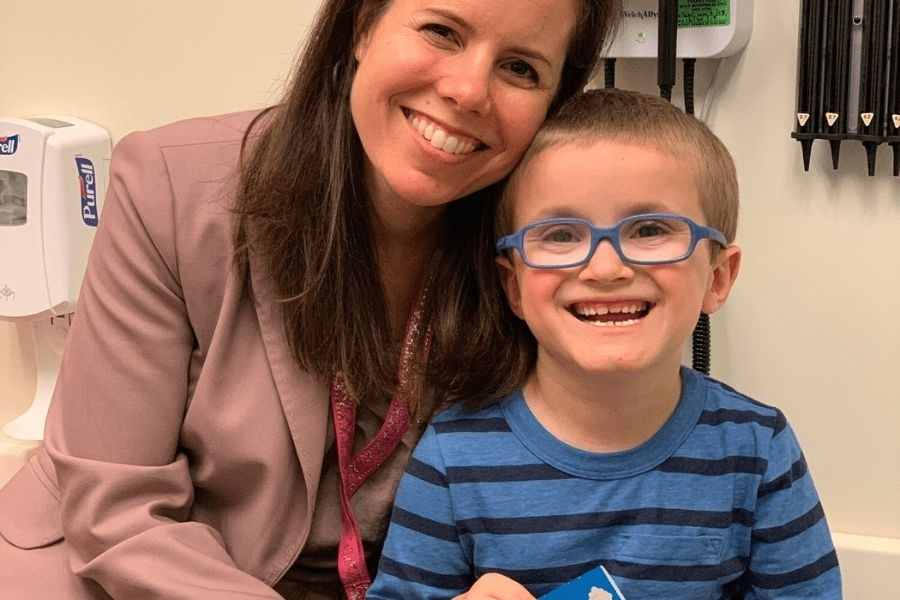
• Alexander's care focuses on addressing long-term complications linked to his condition.
• These complications encompass seizures, mobility challenges, spasticity, and hypotonia.
• Additional concerns include scoliosis, obstructive hydrocephalus, and dysphagia.
• Gastrointestinal symptoms like vomiting, reflux, and failure to thrive are also managed.
• Urinary retention is another aspect of care requiring attention.
• It's noteworthy that symptom severity may fluctuate during the treatment process.

The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
Know more about
Our Healthcare Planner
Personal Health Planner at BNC is a support staff who listens to your concerns and connects you with a Neuro Care provider. They prioritize your needs and create a trusting relationship between you and the provider.
Three fundamental values we can assure you:
1. Personalized Healthcare.
2. Most advanced robotic therapies
3. Transparent pricing